In this 99th edition of the Research Digest, we highlight the discovery of WASF3, a key protein linked to exercise intolerance in ME/CFS. We also explore the use of health survey tools to better convey the burden of ME/CFS in Australia. Additionally, we delve into the analysis of plasma samples, identifying promising metabolites for diagnosing long COVID. The digest concludes with personal accounts from individuals affected by ME/CFS, echoing Anne Wilson’s (CEO of Emerge Australia) call to action to address the healthcare system’s oversight of ME/CFS patients.
Contributing Digesters: Solène and Sophie. Digest Editor: Simone Eyssens
You can also join our community and choose to have the Digest delivered straight to your inbox at the end of every month, by signing up to our mailing list here.
We appreciate the support of everyone who reads the Digest – we encourage regular subscribers to support us with a monthly suggested donation of $2.
WASF3 disrupts mitochondrial respiration and may mediate exercise intolerance in myalgic encephalomyelitis/chronic fatigue syndrome
Authors: Wang PY, Ma J, Kim YC, Son AY, Syed AM, Liu C, … Hwang PM (National Institutes of Health, USA)
Publication: Proceedings of the National Academy of Sciences
Link: http://www.pnas.org/doi/10.1073/pnas.2302738120
The aim of this study was to understand the cause of fatigue and exercise intolerance, in a 38-year-old woman with post-cancer fatigue. The authors then investigated whether fatigue and exercise intolerance shared a common pathophysiology, by applying their results to people with ME/CFS.
The 38-year-old woman with post-cancer fatigue and exercise intolerance (S1) was studied alongside her 34-year-old brother, who did not experience fatigue (S2). Both participated in a submaximal foot exercise test, followed by magnetic resonance spectroscopy to examine muscle recovery, as defined by replenishment of phosphocreatine (PCr). The authors found that muscle recovery took considerably longer in S1 (80 seconds) compared to S2 (30 seconds).
Further analysis revealed over-expression of Wiskott–Aldrich syndrome protein family member 3 (WASF3) in S1’s cells compared with S2. When WASF3 expression in S1’s cells was reduced, oxygen consumption increased, as a sign of increased mitochondrial function. In addition, mice with induced WASF3 over-expression displayed reduced exercise capacity and reduced mitochondrial function. Furthermore, muscle biopsy samples taken from 14 people with ME/CFS showed significantly elevated WASF3 compared to healthy controls. Taken together, the authors conclude that these results suggest that WASF3 may play a role in exercise intolerance in conditions like ME/CFS.
Given the importance of endoplasmic reticulum (ER) and mitochondria interaction in muscle function, the authors propose that ER stress may regulate WASF3 in muscle cells and disrupt cellular respiration. They also propose that this may provide a mechanism to understand exercise intolerance as observed in both S1 and people with ME/CFS and long COVID.
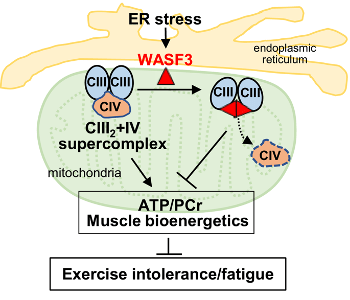
Figure: A proposed model of how WASF3 regulates mitochondrial function. Endoplasmic reticulum stress induces WASF3 to interact with Complex III subunits and its physical presence prevents the assembly of supercomplex III2+IV. The disruption of mitochondrial supercomplex by WASF3 reduces oxidative phosphorylation, which could result in symptoms such as exercise intolerance and fatigue.
Assessing health state utilities for people with myalgic encephalomyelitis/chronic fatigue syndrome in Australia using the EQ-5D-5L, AQoL-8D and EQ-5D-5L-psychosocial instruments
Authors: Orji NC, Cox IA, Jason LA, Chen G, Zhao T, Roberson MJ, … Campbell JA (University of Tasmania, Australia)
Publication: Quality of Life Research
Link: http://link.springer.com/article/10.1007/s11136-023-03498-8
Health state utilities (HSU) measure a person’s preference for a particular health state and are measured on a scale from zero to one, where zero represents death or states equivalent to death and one represents ideal health. HSU have been shown to be independent predictors of patient outcomes, and when combined with measures of health-related quality of life (HRQoL) can be helpful for clinical assessment, relationships and management. The aim of this study was to investigate HSU and establish a multi-attribute utility instrument (MAUI) for Australians with ME/CFS.
The study included 198 Australian participants who self-reported a diagnosis of ME/CFS. Participants undertook an online survey to assess the human and economic impacts of ME/CFS. The survey included questions on disability and fatigue severity from the De Paul Symptom Questionnaire, as well as three HRQoL instruments (AQoL-8D, EQ-5D-5L and EQ-5D-5L-Psychosocial) which measure a wide range of factors, including mobility, pain, depression & anxiety, community connectedness.
The average HSU was similar across all three HRQoL instruments (0.44-0.46), almost half that of the general population (0.77-0.89). Younger participants (under 45) had lower HSU than older participants (over 45), which is the opposite of what is found in the general population. Finally, as disability and fatigue increased, HSU decreased significantly, which is consistent with studies into other disabling conditions, like multiple sclerosis.
Analysis of the three HRQoL instruments found that the results were interchangeable. Based on this, the authors recommend the use of the EQ-5D-5L-Psychosocial for future studies, to ensure the least participant burden.
The authors conclude that these results highlight the significant impact of ME/CFS on the HRQoL of those who live with the condition.
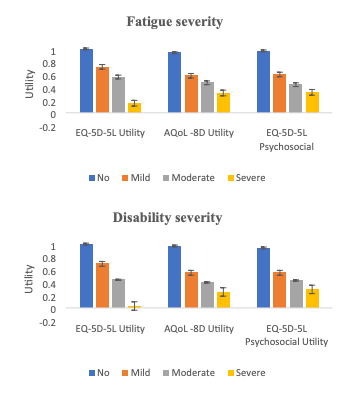
Figure: Mean HSU based on fatigue and disability severity
The plasma metabolome of long COVID patients two years after infection
Authors: López‐Hernández Y, Monárrez‐Espino J, García López DA, Zheng J, Borrego JC, Torres‐Calzada C, … Wishart DS (University of Alberta, Canada)
Publication: Scientific Reports
Link: http://doi.org/10.1038/s41598-023-39049-x
An estimated 30% of patients who experience a COVID-19 infection will develop long COVID (long-term health problems following an initial COVID-19 infection). In this study, the authors’ goals were (1) to identify long-term metabolic changes in long COVID patients which could be utilised as diagnostic biomarkers, and (2) to measure immunity markers.
Participants were recruited from patients with a COVID-19 infection admitted to either of two hospitals in Mexico, between March and November 2020. Participants included 15 participants who had paired plasma samples from acute COVID-19 and post-COVID phases, and 33 participants had clinical information and plasma samples from the post-COVID phase. To assess the severity of long COVID, all 48 patients underwent diverse tests to assess their symptoms. Participants were then divided according to their reported symptoms into the following 3 categories: (1) Recovered (18 patients with no persistent symptoms), (2) long COVID Class A (18 patients reporting less than 5 persisting symptoms), and (3) long COVID Class B (12 patients reporting 5 persisting symptoms or more). Plasma samples from 37 individuals testing negative for COVID-19 and collected in 2020, served as negative controls. The authors used a combination of LC–MS/MS (Liquid Chromatography with tandem Mass Spectrometry) and FIA MS/MS (Flow Injection Analysis tandem Mass Spectrometry) to quantify 108 metabolites in available plasma samples. They also used an immunoenzymatic assay to measure IL-17 and leptin. The comparison between paired acute COVID-19 and long COVID samples revealed 53 statistically different metabolites. Thecomparison between long COVID and controls revealed 27 metabolites that remained dysregulated in long COVID even after two years. Glutamine/glutamate ratio was significantly increased in long COVID patients and may explain the neurological symptoms while lactate/pyruvate ratio was decreased. The best variables to differentiate controls from long COVID were phenylalanine, glutamine/glutamate ratio, taurine, and glutamine.
The lactate/pyruvate ratio, lactate, arginine, and the ornithine/citrulline ratio were the best variables to differentiate long COVID Class A (fewer than 5 symptoms) from long COVID Class B (5 or more symptoms). The lactate/pyruvate ratio was best able to differentiate long COVID Class B from long COVID Class A and Recovered patients. IL-17 was significantly increased in long COVID Class B relative to Class A, and relative to Recovered patients. Leptin levels were not statistically different between the three groups.
The authors conclude that lactic acid, lactate/pyruvate ratio, ornithine/citrulline ratio, and arginine are the most relevant metabolites to identify patients with complicated long COVID in their study. They recommend these biomarker candidates undergo further validation in larger and heterogeneous populations.
I’ve never met some of my closest friends and it’s likely I never will
Authors: Hodgins H
Publication: ABC Everyday
Link: http://www.abc.net.au/everyday/never-met-some-of-my-closest-friends/102626616
Meeting new people is challenging when you’re housebound or bedbound due to chronic illness. And trying to maintain contact with healthy friends, who may not always understand chronic illness, can also be an extremely lonely and isolating experience to navigate.
In this article, the author reflects on how social media can be a powerful tool for developing meaningful friendships with others in similar situations. The author notes that, in online “clip-spaces”, vulnerability is not misunderstood by others, making it safe to be vulnerable. She describes experiencing a feeling of “lightness” and the experience of days becoming better as a result of the support she accesses through her friends in the online disability community. The author challenges the socially held idea that online relationships are less meaningful than in-person relationships. She suggests that equating being “chronically online” to a character flaw, dismisses the unique value online spaces hold for disabled people. She concludes that social media can be understood as a “great equaliser” in that it enables friendships that transcend boundaries related to place, class, and ability.
Why myalgic encephalomyelitis/chronic fatigue syndrome is nothing like everyday tiredness
Authors: Young E
Publication: ABC News
Link: http://www.abc.net.au/news/2023-09-09/why-mecfs-is-nothing-like-everyday-fatigue/102776070
In this article, the author aims to explain the devastating impact of ME/CFS on those living with the condition.
Dee, a former psychologist and lawyer who lives with ME/CFS, says it’s like “having lead weights attached to my limbs … or being pulled down by gravity”, and like “waking up on low battery every day … and being a prisoner to my body’s limitations.” She describes post-exertional malaise as like quicksand, in that the harder she pushes to try and do things, the worse she becomes.
Zoe Cutcher, former epidemiologist, says that not being able to take her kids to the park or participate in school activities like Book Week has been especially difficult. They miss out on having me go out on adventures with them,” she says. “You just have to shrink your world down to the size where it’s safe to live.”
Anne Wilson, CEO of Emerge Australia, said that the invisible nature of the condition meant that, even though symptoms are so debilitating that people can’t “continue with the rest of [their] life: to work, to earn money, to continue [their] studies, to continue to go to school, for parents to continue to parent,” they’re not believed because the symptoms can’t be seen. Anne says that people with ME/CFS cannot continue to be ignored in the health system.

