HealthPathways are clinical management and referral resources designed to be used during consultations with GPs. Each area in Australia has a Primary Health Network (PHN) that adapts a HealthPathway to make it relevant to their local health services.
In 2023, Emerge Australia partnered with the North Western Melbourne Primary Health Network to develop a HealthPathway for ME/CFS (Myalgic Encephalomyelitis/Chronic Fatigue Syndrome).
Early diagnosis ensures patients receive management that may reduce the risk of their condition deteriorating. It also enables referral for vital support services and provides answers for the patient and their loved ones.
Patients with long COVID who present with post-exertional malaise (PEM) should have ME/CFS included in the differential diagnosis as the presence of PEM may change activity and exercise advice.
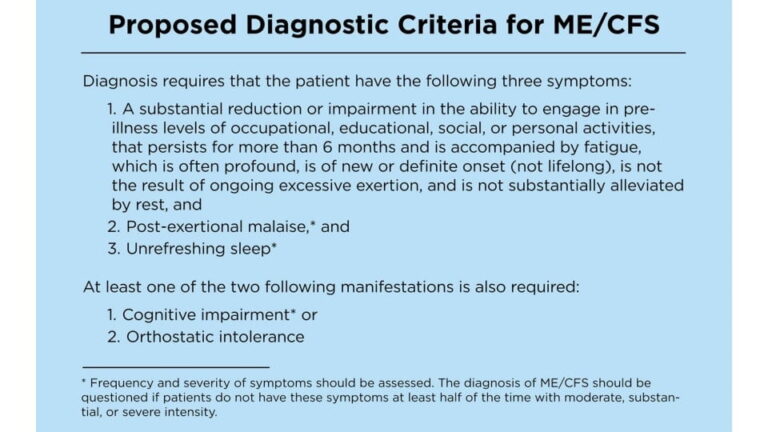
National Academy of Medicine clinical criteria
The National Academy of Medicine (NAM) criteria [1] are recommended for clinical settings by the Centers’ for Disease Control (CDC) and Emerge Australia, as they were designed for diagnosis in the clinical setting.
Other common symptoms include, but are not limited to:
- muscle pain
- joint pain without swelling or redness
- headaches of new type, pattern or severity
- swollen or tender lymph nodes
- frequent or recurring sore throat
- feeling cold or hot, may include night sweats
- light, sound or olfactory sensitivity
- chemical sensitivity including sensitivity to medication
- gastrointestinal and genitourinary symptoms
- muscle weakness, that may fluctuate.
If a patient is presenting with signs and symptoms that raise the possibility of ME/CFS or long COVID, it is important they rest and pace their activity while a diagnostic workup occurs. Advising patients to engage in activity that provokes symptoms is no longer recommended. – NICE Guidelines (2021) [2].
Diagnosing ME/CFS may take several visits. Discuss with your patient how best to balance multiple medical visits with their energy limitations.
Keep in mind some patients may not appear unwell during clinic visits, but recovery time may be required. More severe patients may not be able to leave the house, even for medical appointments.
Paediatric and adolescent ME/CFS diagnosis
The current diagnostic criteria for paediatric and adolescent ME/CFS are available here:
“Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Diagnosis and Management in Young People: A Primer”
Laboratory Tests
While there are no diagnostic tests sensitive and specific enough to diagnose ME/CFS, tests can look for other conditions, or guide clinical management. A list of routinely performed tests can be found here.
Functional Impairment
Significant reduction in capacity compared to pre-illness function is always present in ME/CFS. This may fluctuate and it will be individual.
Establishing your patients’ patterns of activity can be a useful insight into the impact of their symptoms. You and your patient may find it helpful for them to keep track of their activity and symptoms for a week or two, to review at their next appointment.
Documenting functional impairment in the medical record has several benefits:
-
- Establishes a baseline to assess the impact of treatment and management
- Provides crucial evidence for claiming Centrelink benefit, NDIS support, income protection or other insurance
- Documenting functional impairment provides evidence of safe activity levels. Safe activity means activity that does not trigger PEM.
The World Health Organization have created a detailed Disability Assessment Schedule (WHODAS) which can be accessed here.
Cardinal Symptom: post-exertional malaise
The cardinal symptom of ME/CFS is post-exertional malaise (PEM). PEM is the exacerbation of symptoms following physical or mental exertion. It can also be triggered by exposure to light/sound/scent.
The level of exertion that will trigger PEM varies according to illness severity and may change over time. Often ordinary, daily activities such as showering, attending a medical appointment, or reading trigger PEM.
Patients may already be pacing activity to avoid PEM. Ask your patient if they are already pacing to manage energy.
Pacing for ME/CFS does not involve gradually increasing activity. Nor does it mean that the person with ME/CFS will be able to do everything they used to be able to do, except slower. It is an energy management strategy that reduces the impact of PEM.
Further distinguishing features of PEM include:
-
- Delayed onset: symptom exacerbation may occur 24 to 48 hours after exertion
- Variable and often prolonged period of recovery to baseline illness severity and symptoms.
Patients may use language such as “crash”, “relapse” or “collapse” to describe PEM.
Unrefreshing Sleep
Sleep may be unrefreshing or there may be circadian rhythm disturbances with day/night reversal. Problems with sleep onset, staying asleep or waking early are also common.
There may be a primary sleep disorder present such as narcolepsy or sleep apnoea and sleep studies may be required.
Patients can use the sleep and pain profile to assess their sleep.
Cognitive Impairments
Most people with ME/CFS have problems with one or more of these areas [3]:
-
- working memory
- attention
- processing speed
- attention deficits
Cognitive impairment may be induced or exacerbated by exertion, both physical or mental. This means that cognitive capacity may fluctuate and has real-world consequences for maintaining employment, study or activities of daily living.
Patients often describe this symptom as “brain fog” or “can’t think straight”.
Allow for this within the consult, and recognise that this may fluctuate. Offer to write things down, and encourage a support person to attend if appropriate.
Orthostatic Intolerance
Orthostatic intolerance occurs when symptoms become worse with upright positions (raised head of bed, sitting or standing) and generally improve when recumbent.
The most common forms of orthostatic intolerance (OI) in ME/CFS are:
-
- Neurally-mediated hypotension (NMH)
- Postural orthostatic tachycardia syndrome (POTS).
However, research suggests symptoms of OI also occur without BP or HR changes [4]. This symptom may be established by careful questioning including:
-
- How do they feel when sitting or standing?
- How long can they sit or stand?
- How does hot weather effect them?
- Do they study or work lying down, in bed or a recliner? Do they prefer to sit with knees to chest or legs under them?
Fainting is not seen in all patients with OI.
Some patients may exhibit dependent acrocyanosis, especially in hot environments like the shower.
OI can be assessed in the office using the NASA lean test, or a referral for a tilt table test can be made. Often, patterns of heart rate or blood pressure changes according to posture can be picked up on a 24 hour heart and blood pressure monitor that may indicate OI.
Orthostatic challenge can bring on PEM and testing may not be suitable for more severe patients.
Exclusionary Conditions
Identify and manage other conditions that may explain symptoms. Once these are treated and stabilised, further consideration of an ME/CFS diagnosis can be made.
Co-occurring Conditions
Co-occurring conditions are common in ME/CFS and do not necessarily rule out an ME/CFS diagnosis. Identifying and managing these may reduce symptom burden [5].
References
1. Institute of Medicine (IOM). Beyond myalgic encephalomyelitis/chronic fatigue syndrome: redefining an illness. (2015).
2. NICE. Myalgic encephalomyelitis (or encephalopathy)/chronic fatigue syndrome: diagnosis and management. (2021).
3. Centers’ for disease control. What are ME/CFS Symptoms. https://www.cdc.gov/me-cfs/pdfs/toolkit/What-are-MECFS-Symptoms_508.pdf.
4. van Campen, C. M., Verheugt, F. W., Rowe, P. C. & Visser, F. C. Cerebral blood flow is reduced in ME/CFS during head-up tilt testing even in the absence of hypotension or tachycardia: A quantitative, controlled study using Doppler echography. Clinical Neurophysiology Practice 5, 50–58 (2020).
5. Bateman, L. et al. Diagnosing and Treating Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). U.S. ME/CFS Clinical Coalition https://drive.google.com/file/d/1SG7hlJTCSDrDHqvioPMq-cX-rgRKXjfk/view (2019).