Welcome to the 98th edition of the Research Digest. This edition features articles that contribute to our understanding of ME/CFS and long COVID. Alongside a Swiss report detailing the experiences of individuals with ME/CFS, the digest presents research on the enduring cognitive effects of COVID-19 and a study demonstrating the advantages of adhering to pacing strategies to accelerate health recovery and improvement.
You can also join our community and choose to have the Digest delivered straight to your inbox at the end of every month, by signing up to our mailing list here.
We appreciate the support of everyone who reads the Digest – we encourage regular subscribers to support us with a monthly suggested donation of $2.
Myalgic encephalomyelitis/ chronic fatigue syndrome (ME/CFS): A preliminary survey among patients in Switzerland
Authors: Tschopp R, König RS, Rejmer P, Paris DH (University of Basel, Switzerland)
Publication: Heliyon
Link: http://www.sciencedirect.com/science/article/pii/S2405844023028025
The authors of this study noted that there is limited data on the disease and demographic characteristics of ME/CFS in Swiss patients. The aim of this study was to examine the demographics, disease history and severity, and burden of disease in a sample of Swiss ME/CFS patients.
The study consisted of 169 individuals with ME/CFS (diagnosed according to the Canadian Consensus Criteria, International Consensus Criteria, or Institute of Medicine criteria) who were members of the ME/CFS association and also Swiss residents. Participants self-administered a questionnaire that included 66 questions relating to their disease history, general demography, therapies, coping mechanisms and the impact of the COVID-19 pandemic.
The majority of participants (72.2%) were women, 76.2% were married/in a partnership, and 34% had no children. The mean age of ME/CFS onset was 31.6 years, ranging from 7 to 69 years.
The study found that Swiss individuals with ME/CFS shared multiple common features. All participants reported profound and debilitating fatigue as a symptom of ME/CFS. More than 90% of participants were able to recall how and when their disease started, with 77% identifying an infectious disease as the triggering event. The majority of participants (82.2%) suffered from comorbidities, the most common being allergies (40.3%), irritable bowel syndrome (35.2%) and migraine (30.2%). The majority of participants listed physical activity (88.7%) and stress (82.8%) as triggers which aggravated their symptoms.
All participants reported a reduction in their activity levels, either at home, at work, or both, with 95.8% indicating a reduction in activity levels of more than 50% compared with pre-illness levels. The majority of the sample were not working or were only working part-time. Fewer than 5% were working full-time. Almost all indicated that ME/CFS was at least partially the reason for their decreased workload. The authors conclude that this study highlights the very high burden of disease of ME/CFS in Switzerland. The authors propose the need for improved knowledge and acceptance of ME/CFS in healthcare and broader society, as well as further research to ensure adequate care for those with ME/CFS in Switzerland.
The effects of COVID-19 on cognitive performance in a community-based cohort: a COVID symptom study biobank prospective cohort study
Authors: Cheetham NJ, Penfold R, Giunchiglia V, Bowyer V, Sudre CH, Canas LS,…, Steves CJ (King’s College London, UK)
Publication: eClinicalMedicine
Link: http://doi.org/10.1016/j.eclinm.2023.102086
Cognitive impairment has been reported after COVID-19 but little is known about the deficits following infection. In this article, the authors investigated (1) whether COVID-19 is associated with cognitive performance, (2) whether symptom duration or ongoing symptoms of COVID-19 are associated with cognitive performance and, (3) whether the association between COVID-19 and cognitive impairment changes over time.
Study participants were volunteers from the United Kingdom COVID Symptom Study Biobank (CSSB), invited to participate in October/November 2020 (Round 1) and May 2021 (Round 2). All participants, comprising 3335 individuals in Round 1 and 2435 individuals in Round 2, with 1768 participating in both rounds, undertook 12 cognitive tasks. Their accuracy, average within-task reaction time, and variation in within-task reaction time metrics were measured. Participants were organized into eight COVID-19 groups for further cognitive performance comparison based on their SARS-CoV-2 test status (negative or positive) and their symptoms (asymptomatic or symptoms lasting less than 4 weeks, 4-12 weeks, or greater than 12 weeks).
The authors found that individuals with a previous positive test at Round 1 had detectable cognitive deficits compared to participants with negative tests. These deficits were more pronounced in individuals with a positive test and whose symptoms had lasted greater than 12 weeks, but were only detectable in individuals who did not feel recovered from COVID-19. Longitudinal analysis of participants in both rounds revealed no evidence of cognitive change over time, suggesting that cognitive deficits persisted.
The authors conclude that persisting symptoms of long COVID seem to be a better predictor of cognitive impairment due to COVID-19 than symptom duration. Longitudinal analysis indicates that deficits for affected individuals persisted for almost 2 years post-infection. Future research should prioritise trajectories and recovery mechanisms from ongoing symptoms following SARS-CoV-2 infection, as well as the long-term implications of the persistent cognitive deficits observed in this study.
The relevance of pacing strategies in managing symptoms of post-COVID-19 syndrome
Authors: Ghali A, Lacombe V, Ravaiau C, Delattre E, Ghali M, Urbanski G, Lavigne C (Angers University Hospital, France)
Publication: Journal of Translational Medicine
Link: http://translational-medicine.biomedcentral.com/articles/10.1186/s12967-023-04229-w
While post-COVID-19 syndrome (PCS) shares many commonalities with ME/CFS, PCS research has not assessed the use of pacing strategies for managing the condition. This study aimed to assess the efficacy of pacing strategies in PCS patients.
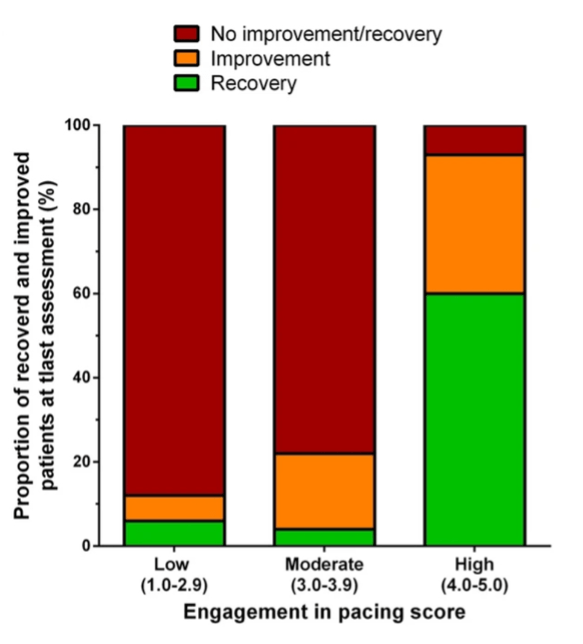
This retrospective study included 86 patients whose PCS diagnosis satisfied WHO diagnostic criteria. Following initial assessments, patients were advised to engage in pacing strategies based on the three pacing pillars. These were defined as staying within energy limits, preventing PEM through identification of PEM triggers, and cautiously increasing activity only once stabilisation of symptoms had occurred. Recovery was defined as the complete remission of PCS symptoms and achievement of pre-illness functionality (including return to work either full or part-time). Improvement was defined as a reduction in either the number or severity of symptoms, but unable to return to work. Based on these definitions, the sample included 29 people who had recovered and returned to work, 20 people who experienced improvement, and 37 people who experienced no improvement. The study involved following up with these people to examine their health status, fatigue and symptom levels, work status and adherence to pacing strategies.
Results showed that PCS patients with high-pacing adherence experienced significantly greater rates of recovery and improvement than those with low or moderate-pacing adherence. Fatigue scores decreased significantly across the three groups between baseline and follow-up, though they were significantly higher in the No Improvement group at follow-up. Pacing adherence was the only variable significantly associated with recovery.
The authors suggest that the beneficial effects of pacing may be due to its ability to support improved functioning across three dysfunctional processes found in ME/CFS patients. These include elevated pro-inflammatory cytokine levels, increased reactive oxygen species, and mitochondrial dysfunction. The authors acknowledge the retrospective nature of this study is a limitation and recommend future prospective trials to validate their results.
Comparison of a 20 degree and 70 degree tilt test in adolescent myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) patients
Authors: van Campen C, Rowe P, Visser F (Stichting CardioZorg, Netherlands).
Publication: Frontiers in Pediatrics
Link: http://www.frontiersin.org/articles/10.3389/fped.2023.1169447/full
Among adults, a 70-degree tilt table test is often used to diagnose orthostatic intolerance via the observation of a reduction in cerebral blood flow (CBF). Previous studies have found higher rates of false positive results in adolescents with ME/CFS during a 70-degree tilt angle. This study sought to determine whether a 20-degree angle was sufficient to provoke a reduction in CBF and haemodynamic abnormalities such as postural orthostatic tachycardia syndrome (POTS) in adolescents, without causing the same level of post-test symptoms as the 70-degree angle.
83 patients aged 10-18 years who attended the Stichting CardioZorg outpatient clinic, experiencing symptoms of orthostatic intolerance, and suspected of having ME/CFS were included in this study. Participants were diagnosed according to the Fukuda and International Consensus criteria and underwent a tilt table test of either 20- (n = 42) or 70- (n = 41) degrees. CBF was measured via extra-cranial doppler measurements.
The authors found that no patients developed POTS at 20-degrees, compared to 32% developing POTS at 70-degrees. CBF reduction of 27% was seen at 20-degrees , with a 31% reduction at 70-degrees. Seventeen participants had CBF measurements taken at both 20 and 70-degrees. Of these participants, CBF reduction was significantly greater at 70-degrees.
The authors propose that these findings demonstrate that a 20-degree tilt angle is sufficient to produce a CBF reduction in ME/CFS adolescents that is similar to the reduction seen in adults at 70-degrees. However, the authors found that these results highlight the need to use the 70-degree angle in adolescents in order to diagnose POTS. They propose that further study is required to determine whether CBF measurements during tilt testing are able to provide an improved method for categorising types of orthostatic intolerance.

